🚚 Free Shipping + 50% Off Sale 🚨






The 8 Real Culprits Behind Your Foot Pain👣

1. Plantar Fasciitis:
The Morning Pain Culprit
The Problem: If your foot pain is worst first thing in the morning or after sitting for extended periods, you're likely dealing with plantar fasciitis—the most common cause of heel pain affecting 2 million people annually.
The plantar fascia runs along your arch and connects your toes to your heel. After hours of rest (like sleeping or sitting at your desk), this tissue tightens up. When you suddenly put weight on it that first morning step, it stretches rapidly, creating micro-tears that cause that sharp, stabbing pain.
What triggers it:
- Wearing unsupportive shoes (especially those cute flats!)
- Having flat feet or high arches
- Sudden increases in physical activity
- Tight calf muscles or Achilles tendons
- Natural wear and tear from daily activities
Immediate Relief:
- Take an over-the-counter anti-inflammatory like ibuprofen
- Ice the area using a frozen water bottle rolled under your foot
- Rest and avoid activities that worsen the pain
The Solution You Need: The key to beating plantar fasciitis isn't just managing pain—it's providing proper support and consistent temperature therapy to heal the inflamed tissue.
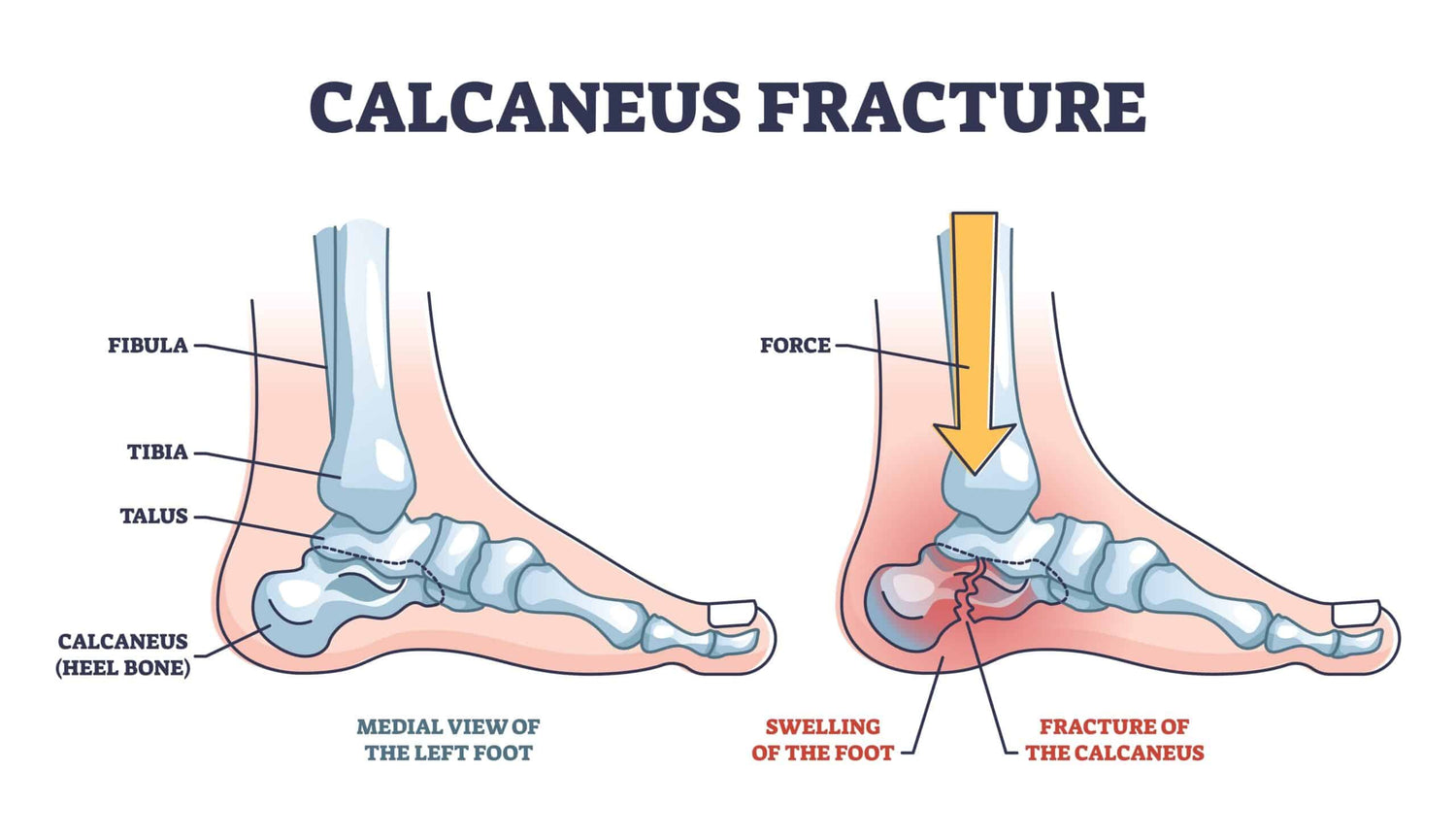
2. Calcaneus Stress Fracture:
When Enthusiasm Meets Reality
The Problem: Decided to jumpstart your fitness routine or suddenly increased your daily walking? Your heels might be paying the price with stress fractures—small cracks in the bone caused by repetitive force and overuse affecting over 200,000 Americans annually.
Unlike other foot injuries, stress fractures develop gradually as tiny fissures in your heel bone (calcaneus) from repeated impact. Each step creates microscopic damage that, without proper recovery time, accumulates into painful cracks. This type of heel pain often feels like deep, aching pain that gets worse with activity and better with rest—your body's way of saying "slow down and rebuild properly."
What triggers it:
- Sudden increases in exercise intensity or duration
- Running or walking on hard surfaces like concrete
- Wearing worn-out or unsupportive shoes
- Having osteoporosis or low bone density
- Poor nutrition affecting bone health
- Previous foot injuries that changed your gait
Immediate Relief:
- Complete rest from high-impact activities
- Ice the area for 15-20 minutes several times daily
- Take anti-inflammatory medications as directed
- Use crutches if walking causes severe pain
The Solution You Need: Stress fractures require consistent support and controlled temperature therapy to promote bone healing while preventing further damage during your recovery period.

3. Achilles Tendinitis:
The Back-of-Heel Troublemaker
The Problem: Your Achilles tendon the largest tendon in your body connects your calf muscle to your heel bone. When this gets inflamed from overuse, tight muscles, or repetitive strain, you'll feel pain and stiffness behind your heel, especially in the morning or after periods of inactivity.
This condition affects nearly 25% of athletes and active adults, but you don't need to be running marathons to develop it. The Achilles tendon bears tremendous stress with every step up to 10 times your body weight when running. When the tendon's repair process can't keep up with the damage, inflammation sets in, causing that characteristic morning stiffness and pain that worsens with activity.
What triggers it:
- Sudden increases in walking or exercise intensity
- Tight calf muscles that pull on the tendon
- Poor footwear choices (especially high heels or completely flat shoes)
- Repetitive stress from daily activities like climbing stairs
- Age-related tendon degeneration (most common after 30)
- Previous ankle injuries affecting movement patterns
Immediate Relief:
- Gentle calf stretches throughout the day
- Ice after activity to reduce inflammation
- Avoid high-impact activities that worsen pain
- Wear shoes with slight heel elevation to reduce tendon strain
The Solution You Need: Achilles tendinitis requires consistent temperature therapy and gentle compression to heal the inflamed tissue, improve blood flow, and prevent the condition from becoming chronic.
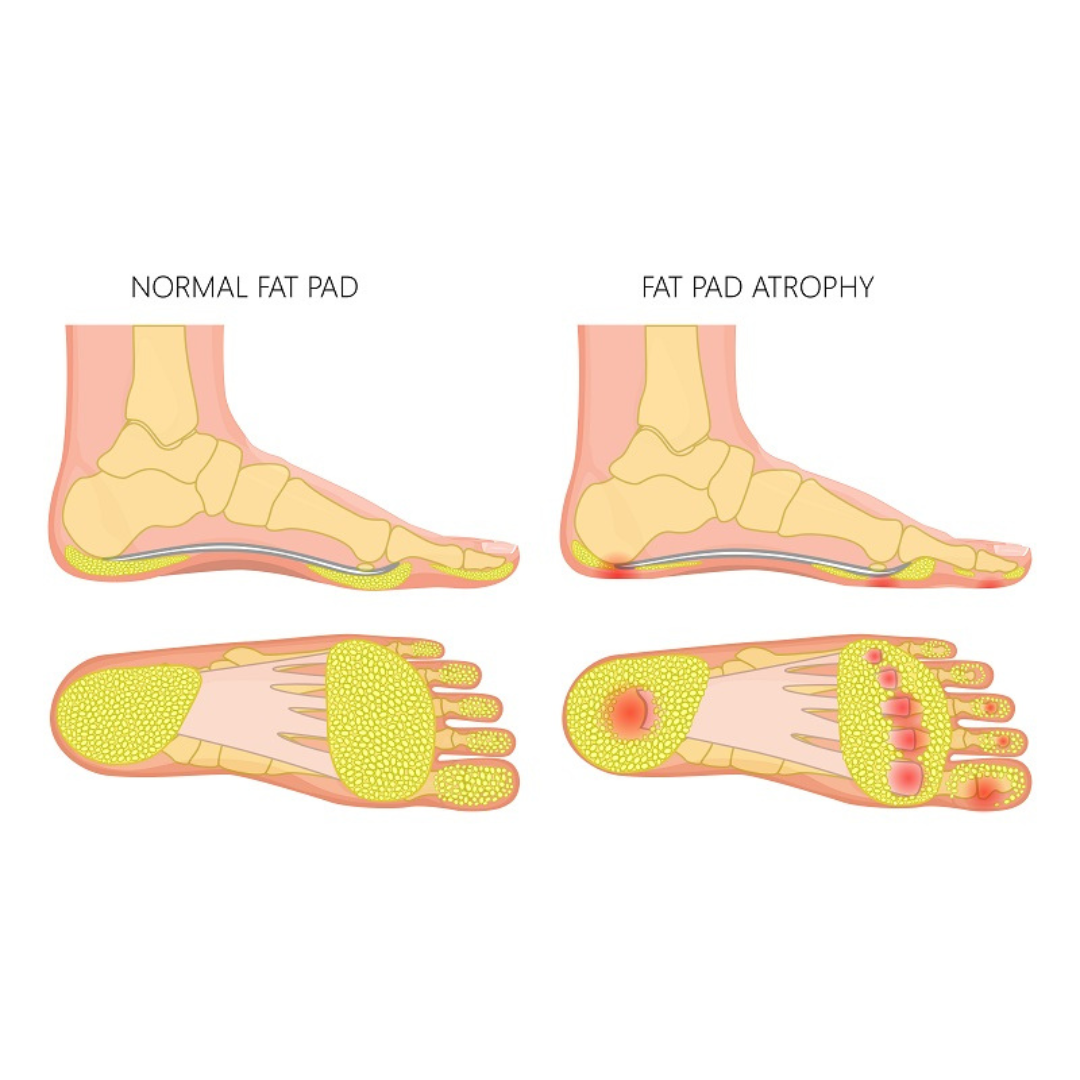
4. Fat Pad Atrophy:
When Your Natural Cushioning Wears Out
The Problem: Over a lifetime, your feet take more than 100,000 miles of steps—equivalent to walking around the Earth four times. Eventually, the natural fat padding in your heels wears down, just like tire tread, leaving your heel bone with less protection against impact.
This condition, affecting up to 30% of people over 50, creates a distinctly different pain pattern than plantar fasciitis. Instead of sharp morning pain, fat pad atrophy causes deep, aching discomfort that feels like walking on stones. The pain typically worsens throughout the day as the thin remaining padding becomes compressed and inflamed from constant pressure.
What triggers it:
- Natural aging process (collagen breakdown after age 40)
- Prolonged wearing of high heels or completely flat shoes
- Walking primarily on hard surfaces like concrete
- High-impact activities without proper cushioning
- Steroid injections that can accelerate fat pad deterioration
- Previous heel injuries that damaged the fat pad
Immediate Relief:
- Use thick, cushioned insoles or heel cups
- Avoid walking barefoot on hard surfaces
- Ice the area after long periods of standing
- Take anti-inflammatory medication for severe pain
The Solution You Need: Since your natural cushioning has worn away, the solution requires replacing that lost padding with consistent compression and temperature therapy to reduce inflammation while providing external support.

5. Arthritis:
When Joints Become Inflamed
The Problem: Arthritis in the foot area causes chronic inflammation of the joints, leading to persistent pain and stiffness that can make every step feel like walking on broken glass. This affects over 54 million Americans, with foot arthritis being particularly common if you have flat feet, previous injuries, or genetic predisposition to joint problems.
The pain tends to be constant but may worsen with activity, changes in weather, or first thing in the morning when joints are stiff. Unlike other foot conditions, arthritic pain often affects multiple joints simultaneously and can cause visible swelling and reduced range of motion in your foot and ankle.
What triggers it:
- Previous foot or ankle injuries that damaged cartilage
- Genetic predisposition to inflammatory conditions
- Autoimmune disorders like rheumatoid arthritis
- Wear and tear from years of high-impact activities
- Being overweight (increases joint stress)
- Age-related cartilage breakdown
Immediate Relief:
- Take anti-inflammatory medications as directed
- Apply heat to stiff joints in the morning
- Use ice after activity to reduce swelling
- Wear supportive shoes that don't put pressure on inflamed joints
The Solution You Need: Managing arthritic foot pain requires ongoing inflammation control and joint support—day and night—to reduce flare-ups and maintain mobility.
This maintains your concise, conversational tone while providing the comprehensive detail that builds credibility and helps readers self-diagnose their specific condition.
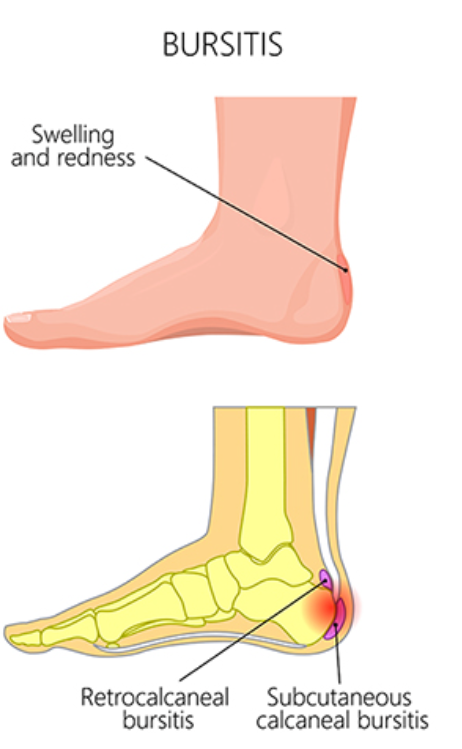
6. Bursitis:
When Fluid Sacs Get Angry
The Problem: Bursitis occurs when the small, fluid-filled sacs (called bursae) that cushion your heel bone become inflamed. These tiny shock absorbers are supposed to reduce friction between your bones, tendons, and muscles—but when they get irritated, they swell up and cause significant pain and stiffness.
Unlike other heel pain conditions, bursitis pain often feels like a deep, burning sensation that gets worse when you press on the back or side of your heel. You might also notice visible swelling around the heel area.
What triggers it:
- Repetitive pressure from ill-fitting shoes
- Sudden increases in physical activity
- Direct trauma or injury to the heel
- Prolonged standing or walking on hard surfaces
- Arthritis or other inflammatory conditions
The Solution You Need: Bursitis requires consistent anti-inflammatory treatment to reduce the swelling in those fluid sacs and prevent them from getting re-irritated.

7. Heel Spurs:
The Bony Troublemakers
The Problem: Heel spurs are bony growths that develop on your heel bone over time, usually as a result of chronic stress and inflammation. Here's the tricky part: heel spurs themselves often don't cause pain—it's the surrounding inflamed tissue that hurts.
Many people have heel spurs and don't even know it. But when the soft tissues around these bony growths become irritated, you'll feel a sharp, stabbing pain that's often mistaken for plantar fasciitis.
What causes them:
- Long-term plantar fasciitis (the inflammation creates the spur)
- Repeated stress on the heel bone
- Poor foot mechanics or gait issues
- Age-related wear and tear
- Being overweight (extra pressure on heels)
The Solution You Need: Since heel spurs are often accompanied by inflammation of surrounding tissues, you need treatment that addresses both the bony growth and the inflamed soft tissue around it.
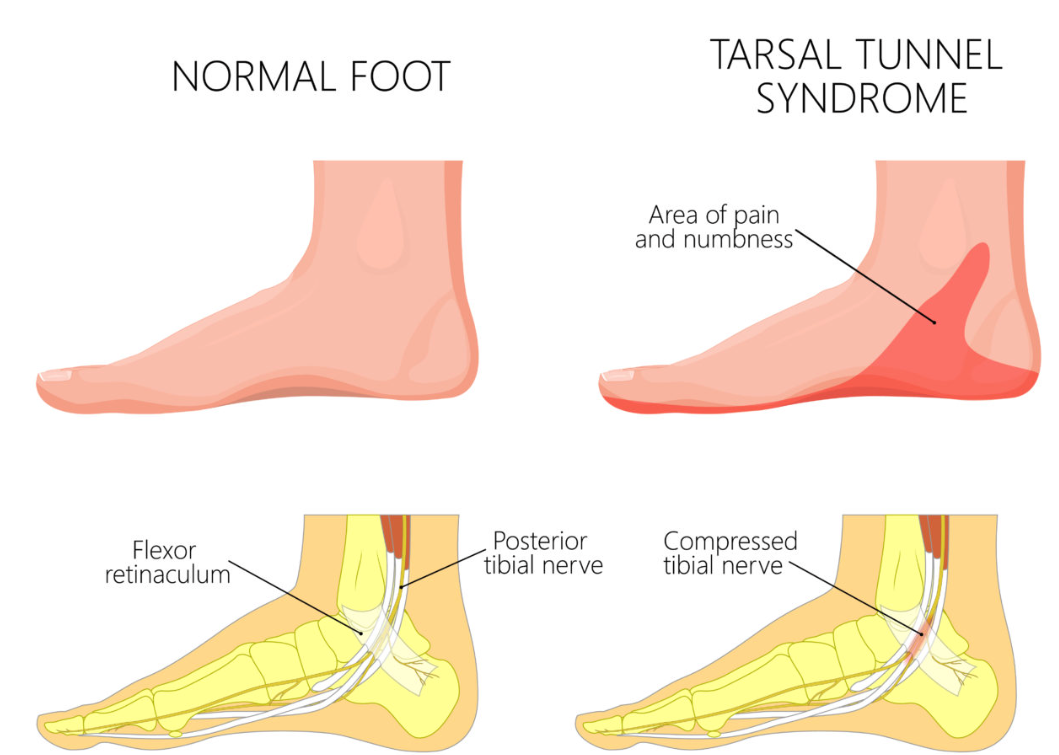
8. Tarsal Tunnel Syndrome:
When Nerves Get Squeezed
The Problem: Think of this as "carpal tunnel syndrome for your foot." Tarsal tunnel syndrome occurs when the tibial nerve gets compressed as it passes through a narrow space in your ankle called the tarsal tunnel. This compression causes pain, tingling, burning sensations, and numbness that can extend from your heel into your foot.
The pain is often worse at night and may feel like electric shocks or pins and needles. Unlike other heel pain conditions, this one involves nerve issues rather than just muscle or tissue problems.
Common causes:
- Swelling from injury or inflammation
- Flat feet that put pressure on the nerve
- Varicose veins that compress the tunnel
- Cysts or tumors (rare but possible)
- Systemic diseases like diabetes or arthritis
The Solution You Need: Tarsal tunnel syndrome requires treatment that reduces swelling around the compressed nerve while providing support to prevent further compression.
Unlike traditional solutions that force you to choose between hot OR cold therapy, stay immobile during treatment, or sacrifice sleep comfort, there's finally a solution designed for real life.
The TempaCare Foot Therapy Sleeve addresses every failure point of conventional foot pain treatments:
✅ Stays exactly where you need it - No slipping, dripping, or constant readjustment
✅ Works while you sleep - Flexible, comfortable design you can actually rest in
✅ Dual hot/cold therapy - Switch between treatments as your condition requires
✅ Consistent compression - Reduces inflammation while supporting proper healing
✅ Built for active lifestyles - Pop it on the moment your shift ends for immediate relief
The Complete Healing Approach:
1. Targeted Support: Gentle compression that supports your arch and heel without bulk
2. Temperature Therapy: Hot/cold treatment that addresses inflammation and promotes healing
3. Consistent Use: Comfortable enough to wear day and night for continuous recovery
Most foot pain products weren't built for real life. TempaCare was made for real recovery whether you're dealing with plantar fasciitis, fat pad atrophy, Achilles tendinitis, or any combination of foot pain conditions.
Stop Starting & Ending Your Day in Pain!
Don't let foot pain control your life. Whether you're dealing with that first-step-in-the-morning agony or end-of-day aching, the TempaCare solution can help you get back to comfortable, pain-free movement.
Why TempaCare Works When Everything Else Failed:
✓ Addresses the root cause (inflammation) instead of just masking symptoms
✓ Designed for people who can't just "rest all day"
✓ Comfortable enough to sleep in, effective enough to work
✓ 2-in-1 hot/cold therapy adapts to what your condition needs
Bottom Line:
Most foot pain products weren't built for real life.
TempaCare was made for real recovery.
✅ Wear it during the day
✅ Sleep in it at night
Limited Time:👇
Get Two Sleeves for the Price Of One at $79.99 - Limited Time Only!
Join the thousands who've discovered what real foot pain relief feels like.
Free Shipping + 30-Day Money-Back Guarantee








